Orofacial Myofunctional Disorders: What are they?
- Ashley Roberts
- Sep 9, 2024
- 3 min read
Updated: Sep 14, 2024
Learn how to define an OMD, recognize the signs and symptoms & what to do next.

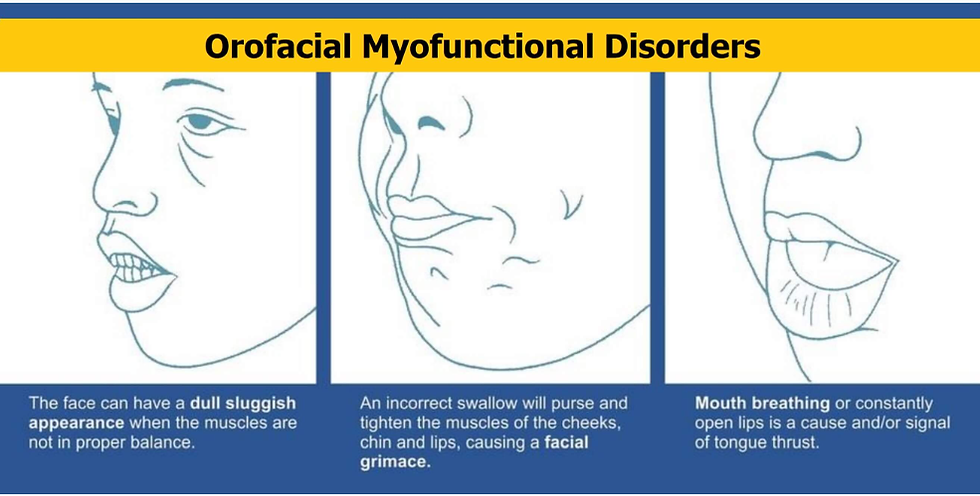
Orofacial myofunctional disorders (OMDs) are abnormal patterns involving the mouth, tongue and facial muscles that interfere with normal growth, development, or function of face, jaw, mouth, tongue, etc. OMDs can be found in children, adolescents, and adults.
OMDs can co-occur with a variety of speech and swallowing disorders. It may be a result of learned behaviors, physical/structural variables, genetic and environmental factors. Let's get into the details.
I started learning more about OMD's when I noticed signs and symptoms in my own mouth and face. Asymmetrical facial features, neck pain, unexplained headaches, and my bite feels uneven when I wake up after wearing my night guard. I entered into my Myofunctional Therapist career knowing I would be my first patient to work on so I can learn to relieve my pain before I help others.
What is an OMD?
Fun Fact, an Orofacial myofunctional disorder is easy to spot once you know what you’re looking for!
If you or your child has a habit of breathing through the mouth instead of your nose, you have an orofacial myofunctional disorder. This can negatively impact your health and physical structures. Thankfully this is not permanent. Through therapy we will eliminate patterns that are keeping you from your optimal wellbeing, and implement exercises to strengthen muscles and retrain the brain to functional movements.
What to look for:
Parafunctional habits: thumb / finger sucking, nail biter, pencil chewing, lip biting, etc
Open mouth at rest or lip incompetence: mouth breathing, chin muscles engaged when lips together
Improper tongue rest posture (tongue lying low in mouth)
Disorders of chewing: only one side, open mouth chewing, no rotation of jaw
Atypical swallowing: forward head movement, neck muscles engaged, tongue thrust pattern aka reverse swallow
What are signs and symptoms of an OMD?
Not just one of these factors means you need to see a myofunctional therapist, OMD’s are multifactorial. Having one could be the reason you have another, therefore causing a chain reaction of signs and symptoms.
|
|

What causes an OMD?
Just like the signs and symptoms of OMD's, the root cause can also be multifactorial. In some cases, it could be a birth defect with a cleft palate, other times its environmental like allergies. Together we investigate the options and find what fits best for you.
Here are some possible causes:
Tongue and lip restrictions ( tongue tied)
Airway restrictions (deviated septum, enlarged tonsils / adenoids)
Changes in feeding habits (breast fed, bottle fed)
Environmental: allergies
Parafunctional habits such as thumb sucking to the point of face structural changes which then leads to mouth breathing and poor tongue rest posture
learned behaviour (never taught to breath through nose / rest tongue up on palate)
What to do next?
If you're concerned about a possible orofacial myofunctional disorder, contact Ashley by email funnyfacemyotherapy@gmail.com to ask questions or set up a 20 minute phone consultation!
If myofunctional therapy is suitable for you, we will collaborate on a regimen of exercises aimed at replacing unhealthy habits with correct muscle function. Together, we will focus on enhancing movement and behaviors to promote improved breathing and overall function.




Comments